In a time where clinicians have more complex decisions to make, and less time to make them in, there needs to be some kind of shortcut to making these calls, right? For years, clinicians have been taught useful tricks to aid their processes and fast decision making, but in recent years another tool has taken the foreground.
Clinical decision tools (also called “CDTs”) have been enabling clinicians to make decisions, such as prescribing or ordering diagnostic tests, in a more efficient manner. These computer-based programmes can be used by healthcare professionals in a wide array of settings and can be especially useful for those who may not have time to consider all the factors involved in making a particular treatment choice including family history, medication availability, as well as patient preference and lifestyle. Aside from clinician timekeeping, they can also improve patient safety by reducing the number of prescribing errors made during the prescribing process, and reduce medical costs.
The challenge of modern medicine
When it comes to prescribing, clinicians face a number of challenges on a daily basis, including:
- Gathering large volumes of information to make an informed prescribing decision.
- The complexity of the choice of medication and its delivery options.
- The need for patient education and counseling on any use of a medication.
- The need for follow-up visits to monitor side effects.
However, there is hope! With CDTs and Clinical Decision Support Systems (CDSS) coming into play, there are more and more stories of technology making these decisions faster, and easier for clinicians facing these pressures.

CDTs are only getting started...
Companies such as OneOme can help pharmacists and clinicians tailor a patient’s medications to their genomic compatibility, reducing the number of unforeseen interactions between a drug, and the patient’s own genomic code.
Going forward, there is also a role to be played by Artificial Intelligence and Machine Learning (AI/ML). But before we get into that, what actually is "AI/ML"?
Simply put, Artificial Intelligence is the simulation of human intelligence in machines. These can then perform tasks that typically require human intelligence. Machine Learning, on the other hand, is a subset of AI that allows the machine to learn from data and from the previous results of recommendations, without being explicitly programmed to do so.
As clinicians, we’re hearing a lot about the power and help that AI/ML will bring, but how? Well, if implemented into a CDSS, it works in the following way:
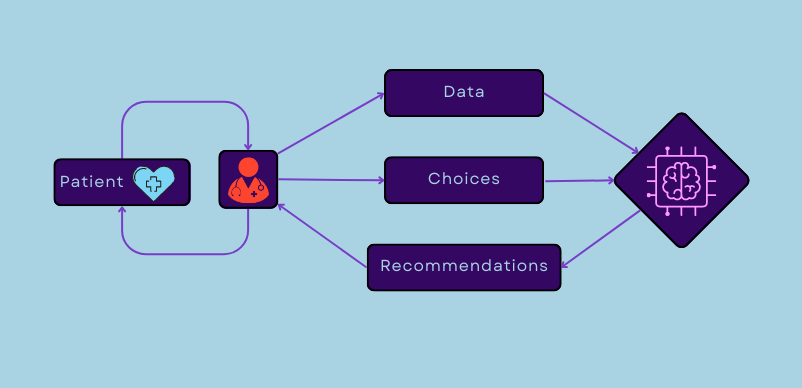 This flowchart shows how CDSS can be used to collate patient data and prescription choices to feedback to the provider to help make better patient recommendations.
This flowchart shows how CDSS can be used to collate patient data and prescription choices to feedback to the provider to help make better patient recommendations.
These can develop into ‘non-knowledge based’ Clinical Decision Support Systems (CDSS), which can interpret vast data volumes in seconds, to provide recommendations based on trends in data sets that may not have previously been observed in clinical practice.
Due to the nature of any system being based on AI/ML, it may then be able to improve its recommendation based on further inputs. Instances of this in action are AI analysing cohorts of CT scans, and determining a patient’s personalised medication risk, technologies that are already being developed by Qure.ai and MedAware respectively.
What about the downsides?
Despite the many benefits that these tools may bring, they do come with their own set of barriers and challenges. Naturally, there are concerns of data privacy. There are failsafe mechanisms to ensure that the data these systems run on is restricted, and limited to consented data sharing, if implemented competently.
Looking more long-term, there is also the concern surrounding the level of dependence; could we reach a point when the clinicians are overly reliant on these tools? Perhaps. One could convincingly argue that there is potential for this to happen all too easily, yet just as avoidable if we look out for it, and now may be the exact juncture that society finds itself at with AI/ML - what is our collective societal mindset towards these technologies, and what questions do we need to be asking as we develop them?
In summary...
Clinical decision tools can be an important tool for clinicians to consider when practising, and some clinicians may not even realise how many they use on a daily basis. They provide evidence-based recommendations in a range of situations, ensuring a more seamless delivery of care. When it comes to contraception prescribing, there is great opportunity for CDTs to benefit patients and clinicians alike, and we hope that our work at Dama Health can help make this opportunity become reality.