What is an ectopic pregnancy?
In order to understand what an ectopic pregnancy is, let's take a step back and think about what we consider to be a "typical pregnancy". When we talk about pregnancies we're usually referring to the 9-month process starting with a sperm fertilising an egg inside of a person AFAB after sex or IVF. This fertilised egg implants into the walls of the uterus to grow into an embryo and, later on in development, into a fetus.
Ectopic pregnancies are different from typical pregnancies. Ectopic means "in an abnormal place or position". Ectopic pregnancy refers to a condition in which the fertilised egg implants outside of the uterus. In over 95% of cases, it will incorrectly implant in the fallopian tubes but there are also cases in which it implants in an ovary or cervix. In all of these cases, the fertilised egg is unable to successfully grow into a fetus and typically won't be able to grow past one trimester. That's because these "abnormal" areas are not like the environment of a uterus. They don't have the vital blood supply a uterus has that can feed the fertilised egg allowing it to grow into a fetus and this is why ectopic pregnancies are often referred to as "non-viable pregnancies".
 ectopic pregnancy in the left fallopian tube
ectopic pregnancy in the left fallopian tube
Since the areas outside of a uterus don't allow for an embryo to grow, there is potential that the area in which the ectopic pregnancy occurs could rupture or hemorrhage. What does it mean when something ruptures or hemorrhages? In the example of an ectopic pregnancy occurring in the fallopian tube, without any intervention the fallopian tube itself could burst (or rupture) and the blood vessels in the surrounding area may be damaged causing unwanted bleeding (or hemorrhaging) inside the abdominal cavity. A ruptured ectopic pregnancy is a medical emergency and will require medical attention.
In the UK, a little over 1% of all pregnancies are ectopic pregnancies. You may think this doesn't sound like a very high percentage however ectopic pregnancies account for maternal deaths each year (around 0.2 deaths per 1,000 ectopic pregnancies in the UK). Ruptured ectopic pregnancies account for around 2.7% of pregnancy-related deaths in the US.
Understanding Ectopic Pregnancy Risk
As the age old saying goes "knowledge is power". When it comes to reproductive health, knowledge can also be empowerment. It's normal to experience fear or anxiety about the possibility or reality of ectopic pregnancies. That's why understanding risk as well as the signs and symptoms of ectopic pregnancy matters.
In a recent study aiming to estimate the rates of ectopic pregnancies among a large sample of women (n=9,256), the researchers split participants into the types of contraceptive methods they used to understand how contraception or lack there of impacts ectopic pregnancies. They found that women using contraceptive methods (listed below) had a much lower risk of ectopic pregnancy compared to women who were not using contraception or were using only barrier methods (such as condoms and diaphragms).
💊
Contraceptive methods included: hormonal IUS, copper IUD, depo injection, implant, oral contraceptive pills, contraceptive patch, or vaginal ring
This is important because there is a common misconception that current hormonal IUS use increases ones risk of getting an ectopic pregnancy. Having a hormonal IUD in place (in addition to the other methods listed above) decreases your risk of ectopic pregnancies compared to no method of contraception or only barrier methods. The misconception comes from the fact that in the rare event that an individual gets pregnant with a hormonal IUS in place, it is more likely to be an ectopic pregnancy than a typical uterine pregnancy.
Some known lifestyle factors that have been reported to increase risk of ectopic pregnancies include: previous ectopic pregnancy, specific sexually transmitted infections, pelvic inflammatory disease, prior fallopian tube or abdominal/pelvic surgery, endometriosis, cigarette smoking, being above 35 years old, and use of IVF. There is different and sometimes conflicting evidence surrounding these risk factors. Many risk factors for ectopic pregnancies are not known and require more research.
Signs and symptoms
Early signs of ectopic pregnancies include: a missed period, positive pregnancy test, vaginal bleeding, stomach or abdominal pain, pain or pressure when going to the toilet, and, in some cases, pain at the tip of your shoulder. Symptoms of an ectopic rupture include: sharp and sudden pain in the lower abdominal area, feeling extremely dizzy, lightheaded and fainting*. Ectopic pregnancies can be treated with medication and, in some cases, surgery.
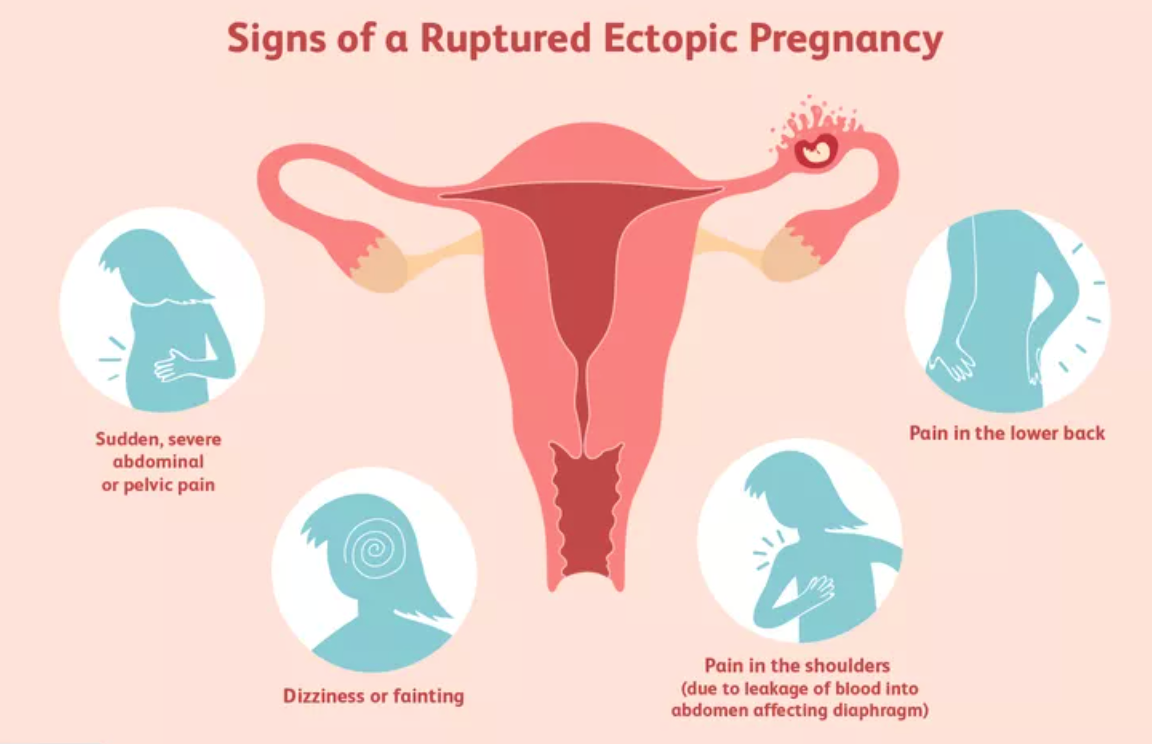 *Call 999 for an ambulance or go to your nearest accident and emergency (A&E) department immediately if you experience these symptoms.
*Call 999 for an ambulance or go to your nearest accident and emergency (A&E) department immediately if you experience these symptoms.
For Support
The Ectopic Pregnancy Trust provides great support for people who have experienced ectopic pregnancies and educational information for everyone. Ectopic pregnancies can have physical and mental impacts that extend even beyond the person affected. The trust provides important resources on helping cope with the impacts that you or someone you know might need.
For those interested in the study details:
Often, rates of conditions in medicine and science can be reported in different ways. Many studies looking to understand ectopic pregnancies aim to measure how many women and people AFAB develop an ectopic pregnancy over a period of time. This can be reported as "person-years at risk" to account for the fact that people are only at risk of developing conditions for a specific period of time.
In this study, they use "women-years" to represent the people at risk (women) as well as the number of people in the study and the amount of time each person spends in the study. They found that women who were not using any contraceptive methods (or just barrier methods) had ~7 ectopic pregnancies per 1,000 women-years. In comparison, women using the hormonal IUD had 0.50 ectopic pregnancies per 1,000 women-years. Less than 1 case indicates that the hormonal IUS and other contraceptive methods below 1 case per 1,000 women-years have protective effects against ectopic pregnancies.