An introduction to cervical cancer
Have a smear test appointment soon, but don't know what to expect? Read everything you need to know in this post.

Gynaecological cancers encompass a range of cancers, including:
- Cervical cancer
- Endometrial cancer
- Ovarian cancer
- Vulvar cancer
- Vaginal cancer
- Uterine cancer
We will be focusing on cervical cancer: what it is, who it affects, the symptoms and the progress in the areas of prevention and treatment.
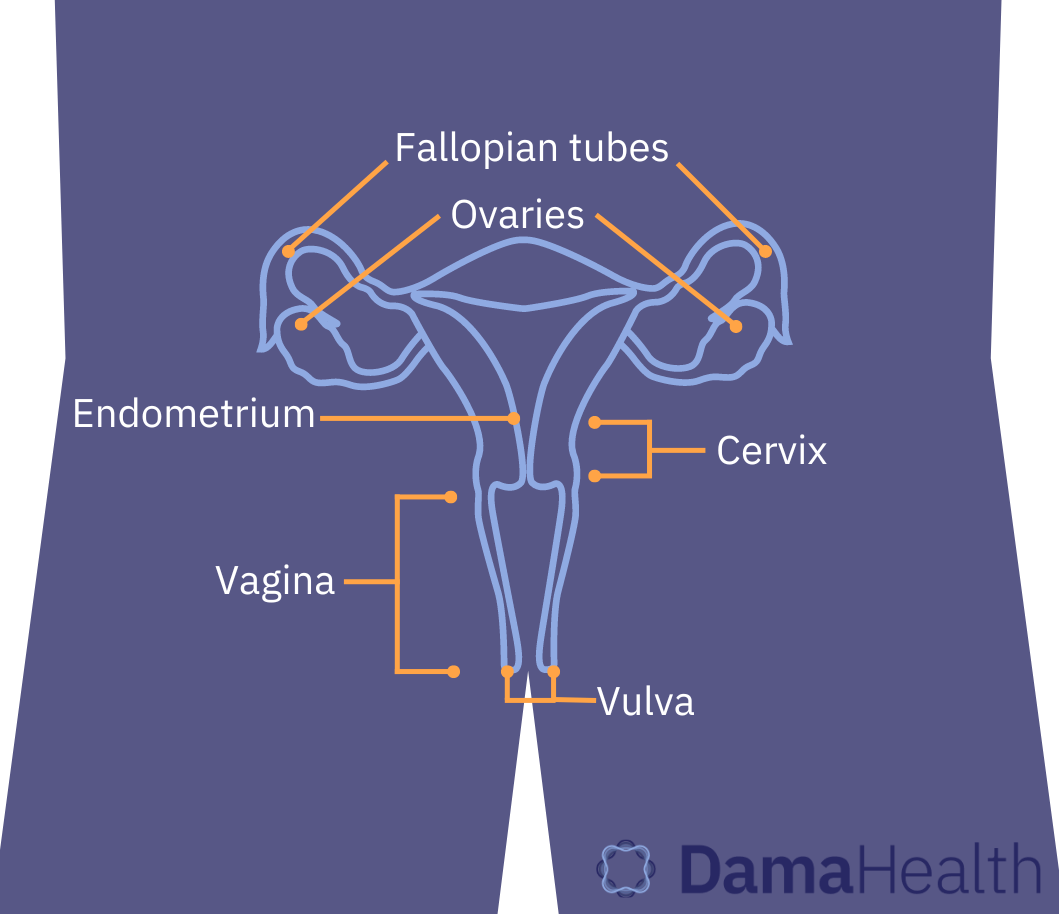
Cervical cancer is a cancer that affects the cervix, the tissue that connects the vagina to the uterus. Data from Cancer Research UK estimates that there are 3,197 new diagnoses of cervical cancer a year and 99.8% of cases are preventable. When cervical cancer does develop, the survival rate is 51% over 10 or more years.
💡
Cervix: The lower part of the uterus, the cylinder-shaped bottleneck of tissue that connects the vagina to the uterus.
💡
Pap smear: A way to collect cells from the cervix, a small brush is inserted into the vagina and used to sweep the walls of the cervix to collect cells
💡
HPV (human papillomavirus): A very common type of virus. People who have HPV usually do not have symptoms however some people develop genital warts. HPV infection can increase the chance of developing cervical cancer.
Early stage cervical cancer does not normally show symptoms, but some symptoms that can appear in individuals include:
- Unusual vaginal bleeding, such as in between periods, during, or after penetrative sex or after menopause.
- Pain/discomfort during penetrative sex.
- Vaginal discharge.
- Pelvic pain (pain in between your hips).
Many of you reading this will probably be thinking, ‘but all these symptoms seem fairly common!’ And you’re right. There are many reasons that could explain these symptoms, such as STI infection, endometriosis or even stress. This highlights the importance of attending your cervical screenings to get your smear test and discussing any changes that are unusual for you with your GP.
What causes cervical cancer?
The most common cause of cervical cancer is Human Papillomavirus (HPV) infection. HPV is the name for a large group of common viruses that affect the skin, and not all of these cause cancer.
There are 12 strains of HPV that can increase risk of cervical cancer. The strains that most commonly cause cervical cancer are HPV16 and HPV18, making up about 70% of cervical cancer cases. HPV is a common virus and, for most of us, our immune systems do the legwork to clear it up quickly before cancer develops. It's like “the common cold that you get in your cervix”. By the age of 50, at least 90% of people with a cervix will come into contact with HPV and only 1% of cases will develop into cervical cancer.
💉
The HPV Vaccine
Two HPV vaccine programmes are running in the UK, one which is offered to all children aged 12 to 13, and the other is for men who have sex with other men.
The first version of this programme used a vaccine called Gardasil which protects against HPV types 16, 18, 6 and 11, which protects against the two most common HPVs that cause cervical cancer, HPV 16 and 18.
The new vaccine Gardasil 9 protects against all of the same HPVs as the Gardasil, but also HPV types 31, 33, 45, 52 and 58.
There are also risk factors (things that increase your chance of developing a disease) for cervical cancer. For example, smoking tobacco is associated with 21% of cervical cancer cases. HIV infection is also associated with cervical cancer in roughly 5% of cases.
- Cervical Cancer Statistics, Cancer Research UK https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer
- Cervical Cancer Symptoms, Cancer Research UK https://www.cancerresearchuk.org/about-cancer/cervical-cancer/symptoms
- What’s causing my spotting in between periods? https://www.livi.co.uk/your-health/whats-causing-my-spotting-in-between-periods/
- What causes heavy or irregular periods? A doctor’s guide https://www.livi.co.uk/your-health/what-causes-heavy-or-irregular-periods-a-doctors-guide/
- Human papillomavirus (HPV), NHS. https://www.nhs.uk/conditions/human-papilloma-virus-hpv/
- Risks and causes - cervical cancer, Cancer Research UK https://www.cancerresearchuk.org/about-cancer/cervical-cancer/risks-causes
- Your guide to HPV, The Royal Mardson https://www.royalmarsden.nhs.uk/your-guide-hpv
- HPV vaccine overview https://www.nhs.uk/conditions/vaccinations/hpv-human-papillomavirus-vaccine/
- Having the HPV vaccine in school, Jo’s cervical cancer trust https://www.jostrust.org.uk/information/hpv-vaccine/school
- Cervical cancer, risks and causes, Cancer Research UK https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer/risk-factors#ref-4
Article edited by Fiona Kennedy, MSc
Medically reviewed by Dr.Paulina Cecula